Malawi Priorities: Maternal and Neonatal Health
Technical Report
Key Messages
While notable progress has been made in Malawi’s efforts to meet the Millennium Development Goals surrounding child health and child survival, progress in curbing neonatal and maternal mortality and morbidity has been less substantial.
Cost-Benefit Analysis run against the most promising singular and sets of interventions within Malawi’s environment revealed two interventions with a significant promise:
- BEmONC5, a compacted set of five specific interventions taken from within the conventional basic emergency obstetric and newborn care package, would target key vulnerabilities facing maternal and neonatal health in Malawi, averting 3,900 stillbirths, neonatal and maternal deaths in 2021, rising annually to 5,800 by 2035. Ensuring that 90% of hospitals and health centers have the necessary equipment, capacity, infrastructure, and medicines to deliver BEmONC5 would require approximately MWK 2.5 billion (USD 3.4m) every two years in investment, put toward staff, training, inventory expansion, medicines, equipment and electricity generators. Through this investment, Malawi would experience a 15% reduction in neonatal mortality, a 5%reduction in maternal mortality and a 13% reduction in stillbirths, enjoying 31 kwacha in social benefits for every 1 kwacha invested.
- Replacing the existing iron and folic acid (IFA) supplements with multiple micronutrients (MMN) 1 for pregnant women would lead to 1300 to 1600 averted stillbirths and neonatal deaths per year. Scaled up to full coverage across Malawi, this program would require an investment of MWK 1.5 – 2.5 billion (USD 2.0m – 3.4m) annually over the next 10 years.
Additional interventions considered in the main analysis include the conventional 15-intervention package of basic emergency obstetric and newborn care (BEmONC) interventions and calcium supplementation in pregnancy. However, these are not as effective uses of resources and would represent less cost-effective uses of limited resources than the above interventions. Further analysis regarding these interventions can be found in the more detailed technical report.
Context
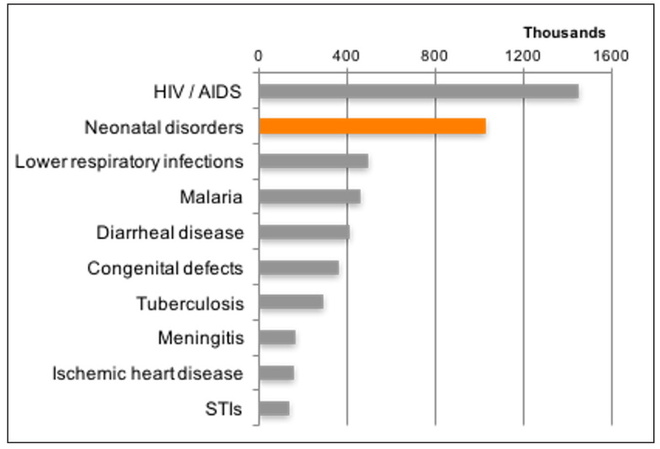
Malawi is one of the few low-income countries to have met its national and international goals for child survival. However, much of the reduction in child mortality has come in the 1-4 age group, and improving newborn mortality remains important. The rate of progress has been less than half of that for overall child mortality, with neonatal deaths at 22 per thousand live births in 2018. Neonatal disorders come second only to HIV/AIDS in terms of years lost due to ill-health, disability, or early death.
Malawi also maintains one of the highest maternal mortality rates (MMR) globally, despite consistent improvements since 2000. In the least developed countries MMR is 427 per 100,000 in 2016. In contrast, Malawi trails behind, averaging 439 deaths per 100,000 births in 2016. The SDGs target a global average of 70 deaths per 100,000 births by 2030.
90% of births are now at medical facilities (either hospitals or health centers) but this has had less impact on maternal and neonatal health than hoped. This is mainly due to the lack of availability of skilled staff (most health centers, where more than half of births take place, have only two nurses and no doctor, for example). Contributory factors include lack of medicines, reliable electricity supply, and a shortage of some items of equipment. This has led to many health centers and to a lesser extent hospital, being unable to deliver key signal functions for BEmONC, or have the resources to effectively provide all 15 interventions associated with the conventional BEmONC package.
Figure 1: Causes of disability-adjusted life years in Malawi, 2017
Additionally, 90% of pregnant women currently take iron and folic acid supplements (IFA), provided during antenatal care (ANC) visits, even if only for relatively short periods. IFA has real benefits since there are a significant number of expectant mothers who are anemic and/or have low levels of folic acid, both of which can lead to poor birth outcomes. While iron and folic acid supplements do have a strong positive impact on MNH writ large, within Malawi, the problem of undernutrition extends further than this, as many women also have inadequate levels of other key micronutrients, such as vitamins A and B12.
Although the country has made considerable progress, a cost-effective program of interventions in maternal and neonatal health would allow Malawi to maximize the impact of allocations toward Maternal and Neonatal Health, increasing the number of lives saved per kwacha spent.
Summary of Findings
The technical report analyzes in detail six potential interventions and/ packages within MNH. For the purposes of this policy brief, we cover only the two most cost-effective ones which may effectively tackle the leading causes of neonatal and maternal mortality in Malawi.
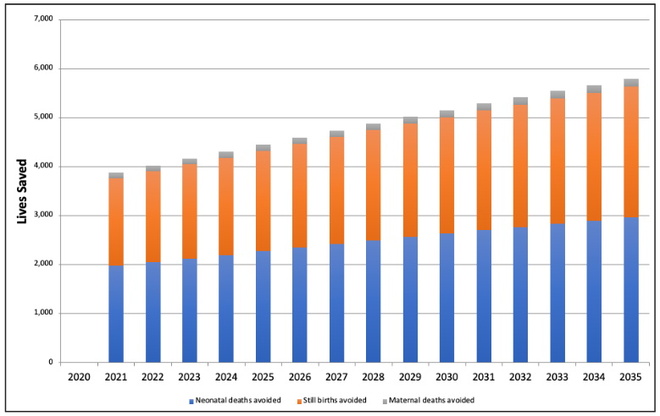
Benefits as Lived Saved
Our examination of the MNH context within Malawi revealed that of the 15 interventions regularly associated with BEmONC, five particular interventions accounted for 90% of the lives saved. The five interventions are: 1) Clean Birthing Environment; 2) Assisted Vaginal Delivery; 3) Neonatal resuscitation; 4) Kangaroo mother care; and, 5) Hygienic cord care. Taken together, these five interventions make a Compacted Obstetric and Newborn Care package which, scaled up to 90% coverage of all hospitals and health clinics, would lead to 1,979 avoided neonatal deaths (15% reduction), 1,787 avoided intrapartum stillbirths (13% reduction) and 107 avoided maternal deaths (5% reduction) in the first year alone. These five interventions do not demand significant further complex equipment or consumables and can be delivered by midwives and nurses (Table 1). Over the period 2020-2035, we expect the scaling up of these 5 interventions alone to save 72,800 lives (Figure 2). The value of these benefits is estimated at MWK 35 billion (USD 47m) in 2021, rising to MWK 125 billion (USD 168m) by 2035, and accrued in the value of lives saved. From a wealth-creation perspective, immediate economic benefits would be generated from averted maternal deaths, however as these represent only 2.5% of the lives saved, most of the economic benefits of this intervention would be delayed until the newborns saved reach working age.
Figure 2: Lives saved from BEmONC5
BEmONC5: A compacted set of five specific interventions taken from within the conventional basic emergency obstetric and newborn care package
Table 1: Five high impact basic emergency and obstetric new-born care interventions
| Intervention | Description | Equipment or consumables required |
|---|---|---|
| Clean birthing environment | A set of simple procedures and protocols to reduce the chance of infection during delivery | Plastic drawsheet, gloves, hand sanitizer or soap and running water, chlorhexidine (antiseptic), cotton swabs, autoclave |
| Assisted vaginal delivery | Vaginal delivery assisted by use of forceps or vacuum extractor | Lidocaine (anesthesia), vacuum extractor or forceps, suture, gauze, syringe, oxytocin, paracetamol, gloves |
| Neonatal resuscitation | An emergency procedure focused on supporting newborn children who do not readily begin breathing | Hand operated resuscitator |
| Kangaroo mother care | Holding of newborn babies with skin-to-skin contact for premature births | Hat and socks for newborn |
| Hygienic cord care | The procedure of cutting the cord with new or sterilized equipment and use of antiseptic on the stump | Chlorhexidine (antiseptic), cotton swab, razor blade, umbilical cord clamp |
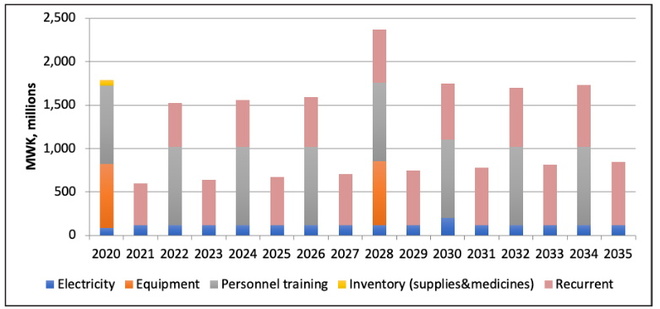
Costs associated with Provision of BEmONC5
Enabling BEmONC5 scaled up to 90% would require investment equivalent to about MWK 2.5 billion every two years with most of the cost required for on-site training including mentorships and recurrent costs associated with delivering the interventions (staff time, consumables, medicines). Additional investments would be needed for autoclaves and back-up electricity sources for facilities. Lastly, to account for stock-outs we include a 30% one-time increase in necessary consumables to act as a buffer. The total estimated investment from 2020-2035 is MWK 19.8 billion (USD 26.6m) and would need to be provided by the government or donor groups. Overall, the targeted package has a benefit-cost ratio of 31. investment from 2020-2035 is MWK 19.8 billion (USD 26.6m) and would need to be provided by the government or donor groups. Overall, the targeted package has an excellent benefit-cost ratio of 31.
Figure 3
Multiple Micronutrients, rather than iron and folic acid supplements
Benefits as Lives saved and improved Lifetime Incomes
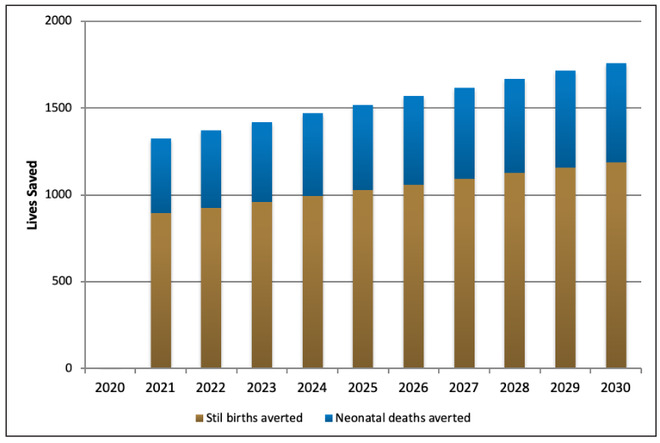
Replacing simpler iron and folic acid supplements with more comprehensive supplements, such as Multiple Micronutrient pills, would improve maternal malnutrition. This intervention would reduce neonatal mortality by 3-4% and stillbirths by 6%, 1,300-1,600 lives annually (Figure 5). It would also reduce prematurity by 5% and low birth weight by 4-5%. These benefits are significant, estimated in the short run as MWK 10 billion in 2021 rising to 21 billion in 2030 from lives saved alone. Additional benefits would accrue to a staggering 47,000 individuals who would avoid being born with low birth weight and 61,000 who would avoid stunting to 2030. Avoiding these afflictions have been shown to raise lifetime incomes by 8% and 43% respectively, a significant wealth creation potential/ economic benefit when these children reach working age. The overall BCR is 14, this intervention offers good cost-effectiveness.
Costs associated with Provision of MMN
Since most women already seek some antenatal care and the health system is set up to provide IFA pills, delivering multiple micronutrients (MMN) in place of IFA is largely a matter of paying extra for the more comprehensive supplements. There is also a modest transitional cost for planning, training and behavioral change communication, but overall the intervention would cost MWK 1,500-2,000 million (USD 2 - 3.4 million) per year (Figure 4). If current arrangements continue, the costs would be financed by the government or donor groups.
Figure 4: Cost of substituting IFA with MMN
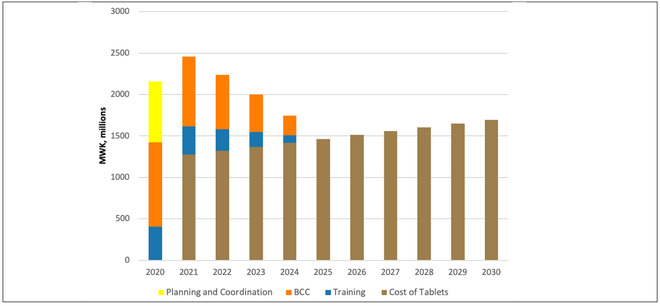
Figure 5: Lives saved from substituting IFA with MMN
Summary Table
| Intervention | BCR | Target group | Impact | Lives saved per year on average | Cost per life saved excluding still births | Additional investment required |
|---|---|---|---|---|---|---|
| Package of 5 high impact BEmONC interventions | 31 Excellent (33% economic benefit; 67% social benefit) | Births occurring in 90% of hospitals and health centers | 15% decrease in neonatal mortality 5% decrease in maternal mortality 13% decrease in stillbirths |
2480 neonates 2240 stillbirths 135 mothers |
MWK 505,000 (USD 680) | Approximately MWK 2.5bn every two years (USD 3.4m) |
| Substituting iron and folic acid supplements with multiple micronutrients | 14 Good (73% economic benefit; 27% social benefit) | All women attending ANC visits | 3-4% decrease in neonatal mortality 6% decrease in stillbirths 5% decrease in low-birth weight |
1040 neonates 500 stillbirths |
MWK 1,050,000 (USD 1410) | MWK 1.5 – 2.5bn per year (USD 2.0m – 3.4m) |
Note: BCRs are based on costs and benefits discounted at 8% (see accompanying technical report). BCR ratings are determined on the following scale Excellent, BCR > 15; Good, BCR 5-15; Fair, BCR 1-5; Poor, BCR < 1. This traffic light scale was developed by an Eminent Panel including several Nobel Laureate economists for a previous Copenhagen Consensus project that assessed the Sustainable Development Goals.
Download the full policy brief here.