Ghana Priorities: Tuberculosis
Technical Report
The Problem
TB is responsible for around 5 percent of total deaths in Ghana annually, and the decline in TB burden is markedly slow, with an average 2.5 percent reduction in TB incidence year on year (GTB 2018). TB mainly affects the working-age population of Ghana (73 percent* incident cases aged 15-44 in 2018), and as many as 70 percent of individuals with TB disease in a given year don’t access TB treatment. For those that are enrolled in treatment, around 15 percent show poor treatment adherence and outcomes, or are lost to follow up. These factors overall resulted in an estimated 15,800 TB-related deaths in 2018.
The program currently estimates that only 32 percent of incident TB cases are notified year on year, and 80 percent of notified cases are enrolled on TB treatment.
To compound this problem, the 2018 WHO Global TB Program report estimated that 16 percent of cases previously treated for TB are resistant to first-line anti-TB drugs, and hence are enrolled on a longer treatment course of second-line anti-TB drugs. A number of these drugs are associated with severe side effects, and these regimens have an overall treatment success rate of only 62 percent (GTB 2018).
Intervention 1: Active Case Finding
Overview
Detection of TB cases in Ghana has historically relied on passive case detection, and more recently the National TB Program has piloted an Intensified Case Finding (ICF) clinic-based TB screening tool, which is now implemented at Outpatient Department Clinics (OPDs) at the national level. Around 6,000 additional TB cases are screened, diagnosed and notified annually through this ICF mechanism, but there still exists a significant proportion of TB cases in Ghana that go undetected. Hence, there is a need to expand the reach of current case finding strategies to find missing TB cases at the level of the community, to detect and enroll on to treatment cases that may otherwise not present at the clinic, or at least not be identified by the health system until presenting with more severe TB disease. TB screening in specific high-risk populations, termed Active Case Finding (ACF), has been demonstrated in Ghana and other settings to yield a significant number of additional cases that would otherwise go undetected (Yuen et al, 2015), refer to the technical appendix for estimates of ACF target population size and TB prevalence.
Implementation Considerations
The intervention focuses on active screening for TB with Chest X-ray in high-risk populations including miners, refugees and their host communities, and in vulnerable urban populations, with an assumed average TB prevalence of 1.5 percent - approximately 5x the national estimate from Ghana’s 2014 National TB Prevalence Survey – across groups totaling 1.6M population. The intervention aims to screen 600,000 individuals in the period 2020-2025, reaching a maximum number of 220,907 individuals screened in 2025- equivalent to 33 percent of total target population (assuming that the overall size of ACF target population doesn't change over time). This coverage target in terms of absolute numbers screened aligns broadly with Ghana’s 2015-2020 National Strategic Plan systematic screening target of screening 60 percent of a target population of 1 million (where the original target year for achieving maximum ACF coverage was 2020).
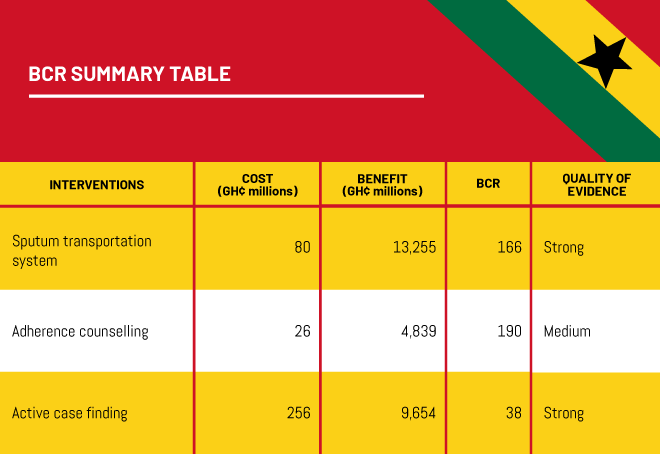
Costs and Benefits
Costs
The unit cost per person screened was estimated at GH¢ 426 based on the 2015-2020 National Strategic Plan and includes patient time, staff time for outreach and household/work visits etc and overhead organization and management as well as screening tools costs. Total costs are GH¢ 2.6m initially rising to GH¢ 62m by 2040. 85% of costs are screening costs with the remainder for additional treatment that arises from improved identification of TB cases.
Benefits
The modelling results indicate that ACF, scaled up over a period of 6 years from 2019 to 2025, would have a significant impact on TB burden and mortality reduction, with 5,022 TB cases averted and 2,221 deaths averted during this period, and 33 per cent of total prevalent TB cases among high-risk groups notified and enrolled on treatment in 2025. Projecting further out, the intervention is estimated to avoid 56,000 TB cases and 26,400 associated deaths from 2019 to 2040.
Intervention 2: Sputum transportation system to improve the accuracy and speed of TB diagnosis
Overview
Coverage of molecular testing among all notified cases in 2018 was estimated at 58 percent (GTB report), up 38 percent from 20 percent coverage in 2017. With the lack of a direct estimate of the numbers of presumptive TB cases tested for TB by GeneXpert i.e. at the primary screening stage of the care cascade, it is assumed that this 38 percent increase in the proportion of notified cases diagnosed by GeneXpert, translates to an approximate 10 percent increase in coverage among all presumptive TB cases. This is reflected in the diagnostic algorithm in the baseline year of the model.
The NTP of Ghana is in the preliminary stages of rolling out a novel sputum transportation system, which aims to provide virtual on-site access to GeneXpert testing for >90 percent of OPD attendants, linking 1,000 health facilities to 126 existing GeneXpert testing sites. This system was initially piloted in the Greater Accra and Western Regions, with planning underway to provide coverage across most/all regions and districts. This would effectively enable TB suspects who provide sputum samples at facilities without a GeneXpert machine onsite, to receive molecular testing for TB without needing to travel to provincial or other more centralized facilities.
Implementation Considerations
In this intervention scenario, we modeled an increase in GeneXpert test coverage at the national level to 90 percent by 2025, to reflect the expansion of sputum transportation and utilization of GeneXpert machines at sites distal from the location of sputum sample collection. We estimate that the coverages of screening through passive case detection and ICF in 2018 were 65.5 percent and 34.5 percent of total screening at the national level, respectively, and in the model, this ratio remains constant during the implementation period
GeneXpert is also used for molecular Drug Sensitivity Testing (DST) in Ghana, with an estimated 100 percent coverage of DST among previously treated cases and 93 percent among new cases in 2018 (GTB report). Expansion of GeneXpert in the model sees a corresponding increase in coverage of molecular DST among new cases to 99 percent by 2025, resulting in an additional 74 MDR-TB case notifications over the scale-up period.
Costs and Benefits
Costs
The rationale behind this intervention is to transport sputum samples to locations where GeneXpert machines are located. The cost of GeneXpert equals approximately GH¢ 176 per GeneXpert test (50 percent of which is transport cost, while the rest includes the labor cost and cost of cartridges and consumables). The cost of sputum microscopy is estimated at GH¢ 12. The cost of drug susceptible TB treatment is estimated at GH¢ 544 while the cost of MDR treatment is calculated as GH¢ 10,400. The intervention costs GH¢ 1.5m initially, rising to GH¢ 17.0m by 2040. Approximately 60% of the costs are for diagnostics and transport, with the remainder for additional treatment.
Benefits
The model predicts that scaleup of GeneXpert over a period of 6 years from the end of 2019 , to 2025, would have a marked impact on TB burden and mortality, with 4,832 TB cases averted and 3,087 TB deaths averted during the period 2019-2025. Projecting further out, the intervention is estimated to avoid 65,000 TB cases and 36,600 associated deaths from 2019 to 2040.
Intervention 3: TB patient education and counseling to improve TB treatment adherence
Overview
The second intervention described above- molecular testing to improve TB diagnostic accuracy and speed- is estimated to reduce pre-treatment loss to follow up (LTFU) and increase treatment enrollment. However, this doesn’t address the problem of defaulters: those patients already enrolled on treatment who are LTFU; and has a relatively small impact on treatment success. TB continues to persist in the country, largely because of patients’ noncompliance with medication (Boateng et al, 2010). Studies in New Juabeng Municipality, Tamale Metropolitan Assembly, and Agogo in Ghana identified patients’ noncompliance with medication as a challenge, as it contributes to the overall sustained burden of TB in Ghana. Multiple socioeconomic factors influence attrition at this point along the TB care continuum; most studies focus on the medical aspects of the disease rather than looking at it from a socioeconomic viewpoint (Yahaya and Acquah, 2013).
This intervention model aims to capture the impact of patient education and counselling on adherence to DOTS and treatment LTFU, as well as on treatment success, based on a meta-analysis of RCTs which test strategies to improve TB treatment adherence (Muller et al, 2018). This analysis identified that among the most effective approaches to improving adherence were DOTS and patient education & counselling. Ghana’s community-based DOTS strategy is well established, and treatment LTFU estimated to be 2.8 percent of all those enrolled on treatment.
Implementation Considerations
In this scenario, we assume that patient education and counselling requires the formation of groups of 6 patients on average, facilitated by a nurse over the course of one hour. Five meetings are held throughout the DOTS treatment regime. The meta-analysis estimates that overall, patient education and counselling with coverage for all cases enrolled on treatment leads to a 13 percent decrease in LTFU, and additionally a 16 percent increase in cure rate (Muller, A. M). The setting of these trials varied, and none addressed the implementation of patient education and counselling specifically in Ghana. Its impact is assumed to be generalizable to this setting.
Treatment success (the sum of patients registered as cured, and completing treatment i.e. without bacteriological confirmation of cure) is represented as a single parameter in TIME, and we assume here that proportions cured and LTFU contribute to an overall increase in the value from 85 percent in 2018 to 85.4 percent in 2025.
Costs and Benefits
Costs
The costs of this intervention include the initial cost of course development, nurse training, nurse time and patient costs. The initial cost of course development is estimated at GH¢ 500,000 and is one off. The direct cost of nurse training is assumed to be GH¢ 2500 per 20 nurses. Future costs of training assume a 20 percent turnover of nurses per year. The cost per nurse hour is estimated at GH¢ 16 – based on actual nurse salaries under TB program. The cost per patient hour (assumed to be full productive time) is taken as GH¢ 3.5 – based on Ghana Priorities standard assumptions. Patient travel costs of GH¢ 1 per meeting per patient are also included while each meeting is assumed to require GH¢ 50 in basic consumables such as stationery or handouts. Total costs of the intervention start at GH¢ 1.6m in the first year rising to GH¢ 4.9m by 2040. Meeting consumables and patient time comprise 39% and 33% of total costs respectively.
Benefits
This intervention has relatively smaller impact on TB burden reduction, compared to the previous scenarios modelled, but is still successful in averting TB cases and deaths. We estimate that the provision of patient education and counselling results in the aversion of 2,654 cases and 999 TB deaths in the period 2019-2025. Projecting further out, the intervention is estimated to avoid 31,000 TB cases and 13,200 associated deaths from 2019 to 2040.